To be more precise, I need is an actual sick day plan. I haven't really had one before. My plan is the past has been "Don't get sick" and that has worked. I think I've had antibiotics once in ten years. For the most past, infections, the flu and colds usually pass me by.
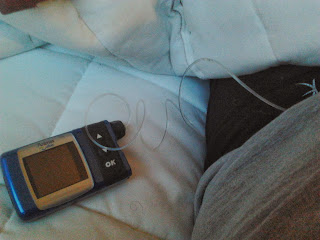
However, not so much with this recent flu/cold/sinus infection. I've felt terrible and my levels have been going sky high and haywire. When my ketones threw out 0.8 I was panicking a little bit.
 |
| Cue: Panic |
The GPs advice was to go to the Emergency Department. I thought this was pretty stupid given they had no idea of my level of ketones or the fact that I was sitting at 0.1 which was in fact within the normal range of ketones. Green even.
 |
| It clearly says that reading under 0.6 mmol/L are in normal range.... |
So, I trusted my gut instinct and didn't seek further medical attention. Reasons why I didn't?
- I was still in normal range - In the green if you will
- I wasn't vomiting
- My levels were high but not super high (10-13mmol/L - am currently running my levels higher to claim back some hypo unawareness)
- The insulin was working (As evidenced that morning with breakfast and the night before when I was at 0.8)
- I wasn't feeling like I was in the onset of DKA, I've been there once and the symptoms aren't something I'm likely to forget
Reasons why I would have gone?
- I had high ketones the night before (0.8) and they showed up the morning after (0.4). That was what was worrying to me.
So I didn't go and was lucky enough to see this number of ketones later in the day:
 |
| Relief |
A couple of days later I emailed my CDE if we could talk sick days at our next appointment and told her about my recent time of it. Her response:
"I think you have managed recent illness superbly well and plan to go to ED if remained ketotic entirely appropriate"
In my own heart I knew that I had acted appropriately, I just felt better when I was reassured that by someone who is a specialist in that area.
I've never really felt much sympathy to people that have colds and coughs. One of the reasons is that I hardly ever get sick so don't really have empathy to their situation. I think the other is that I manage with this chronic medical condition every day and is that when I get sick, where others might be able to wait it out with chicken soup and ice cream, I'll have to go to the Emergency Department to get better. I'd prefer the chicken soup thanks. Hold the ice cream though, not too much of a fan.
How does everyone else manage their sick days? Would love to hear about other experiences :)
S xx